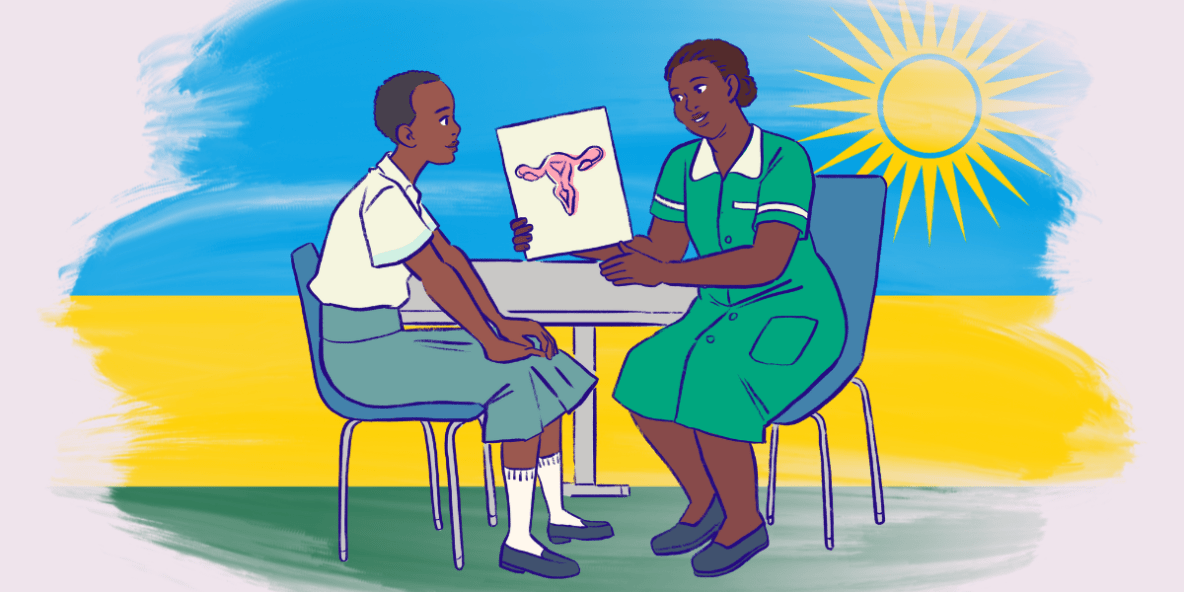
Earlier this month the parliament in Rwanda lowered the legal age for accessing reproductive health care from 18 to 15 years old. This means that young people from 15 onwards will no longer require parental consent to get contraception from a medical facility.
This change has come about with the aim of removing barriers that prevent young people from making informed, timely decisions about their bodies. This ruling comes in response to the persistent rise in teenage pregnancies, unsafe abortions, and missed opportunities for care. It reflects the reality that young people are already navigating these challenges without adequate support.
As Medical Doctors for Choice (MDFC) we are pleased to see the Government taking this important step towards recognising the realities of young people’s lives and increasing their access to potentially life-saving healthcare.
What does the ruling mean for young people in Rwanda?
We are awaiting a ministerial order with further information from the Ministry of Health, but we do know that under this new law, adolescents can now access:
- Comprehensive sexuality education (CSE)
- Menstrual health support
- Contraceptive services
- HIV and STI screening services
This matters because it removes a major barrier to care for young people. It respects their right to make informed decisions. And it helps to prevent unintended teen pregnancies and reduce risks from unsafe abortions.
Additionally, this law opens the door for digital health solutions through its Digital Health Regulation. While sexual and reproductive health services in Rwanda have traditionally required in-person visits, this reform creates space to advocate for and implement digitally enabled interventions. This could include telemedicine for safe abortion care, online contraceptive counseling, virtual SRHR consultations, and other remote support services. It signals a shift towards integrating technology into SRHR delivery, expanding access and reducing access barriers, especially for young people and those in underserved areas.
How did this legal change come about?
This change didn’t happen in a single parliamentary sitting. It was years in the making, driven by the persistent advocacy work of civil society voices, most importantly the Rwanda SRHR Coalition, of which MDFC is a founding member. Through the Coalition, we were actively engaged in raising the need for improved adolescent care through participation in parliamentary discussions, as well as playing our part in shifting public opinion over the past five years.
Back in 2011, the Ministry of Health issued an Adolescent Sexual and Reproductive Health and Rights Policy, acknowledging rising teen pregnancy rates and the need for youth-friendly reproductive health services. This policy called for improved sexuality education, adolescent-friendly corners at health centers, and outreach to youth. However, it remained a policy guideline; minors’ access to services was still constrained by law (parental consent was generally required for those under 18).
A milestone came in May 2016 when parliament passed the first comprehensive reproductive health law. The law affirmed that any person who has attained majority (18 years) has the right to make decisions regarding their own reproductive health, “subject to provisions of other laws”. However, the law effectively left in place the requirement that those under 18 obtain parental consent for most reproductive health services.
In the same period, Rwanda was also reforming its abortion laws. A 2012 revision of the Penal Code Law and a 2019 Ministerial Order allowed abortion under limited exceptions (rape, incest, forced marriage, or risk to health), and in 2018, the law was further liberalized, removing the requirement of a court order and permitting doctors to approve legal abortions in the defined circumstances.
By the late 2010s, Rwanda faced a worrying rise in adolescent pregnancies, which kept SRH for minors in the national spotlight. The percentage of girls who have begun childbearing increased from approximately 4% in 2005 to over 7% by 2015, and continued to rise. Civil society organizations and youth advocates became more vocal in urging the government to remove barriers that prevented adolescents from protecting their health. They urged that the strict age of 18 for accessing services was contributing to the teen pregnancy epidemic by disqualifying sexually active teens from contraception and even from accurate sexual education at the health facilities. By 2019-2020, calls to lower the age of consent for SRH services had gained momentum, setting the stage for legislative action.
In October 2022, Parliament rejected the teen contraceptive bill. Cultural and religious opposition heavily influenced this outcome: Parliamentarians raised concerns that enabling 15-year-olds to obtain contraceptives might encourage teenage promiscuity and undermine Rwandan values. This parliamentary defeat in 2022 revealed a temporary setback in addressing the legal age of consent for SRH services. Yet it also galvanized public debate. Media coverage and social media in Rwanda saw an outpouring of opinions, with many youth advocates and civil society organizations urging lawmakers to reconsider. The issue did not disappear; instead, it set the stage for revisions in the near future under a broader health law reform.
After years of preparation, debates, and persistence, Rwanda Ministry of Health ushered in a major reform of its health legal framework. On August 4th, 2025, the Chamber of Deputies passed the health service bill, a comprehensive law governing healthcare services in Rwanda. It consolidates and updates several previous laws into one modern statute. It introduced an array of innovations in healthcare delivery, but most relevant, it addressed the longstanding gaps in sexual and reproductive health rights. Key areas reformed in this law include: Digital Health Regulation, Assisted Reproductive Technology (ART), Lowering the Age of Consent to access health services, Mental health inclusion, telemedicine recognition, and Protecting patients’ rights.
What will the impact of this legal change be?
In practice, this change opens doors, but it doesn’t automatically mean services will be accessible, stigma-free, or evenly available across Rwanda. The legal victory is a foundation. Turning it into real-world access requires the kind of systems change, provider training, and policy alignment that MDFC works on every day.
The law is a breakthrough, but it is not the finish line. MDFC sees it as the foundation for tackling the deeper operational and institutional barriers that remain. In many health facilities, for example, unlawful internal policies still block safe abortion despite the ministerial order that progressively expands the right to abortion, and the expanded mandate for health centers remains unusable without telemedicine.
Through our SAAF-supported work, boosted with this recent bill, we are addressing these gaps directly, advocating for hospital policy reforms so they comply with the law, and building telemedicine pathways to make abortion care possible in health centers. Our goal is to ensure these legal rights are backed by functional systems, trained providers, and community awareness so that no one is denied care they are entitled to receive.
By Richard Mbazumutima, Director of Programs, Education and Research at Medical Doctors For Choice (MDFC) – a SAAF grantee partner in Rwanda.